Ivaylo Tzvetkov, Krasimir Shopov, Jordan Birdanov, Ivan Jurukov,
Hospital Doverie, Sofia, Bulgaria
Background
• According to recent studies obese patients with type II diabetes who undergo bariatric surgery revert to normal blood glucose and insulin levels and develop a dramatic increase in insulin sensitivity.
• However, the mechanisms involved are unknown.
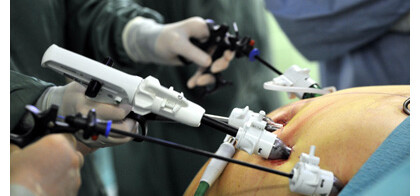
• The Bariatric procedures, which develop such a rapid decrease in blood glucose and insulin levels are the malabsortive procedures as gastric by pass, duodenal switch and bilio-pancreatic diversion.
• Laboratory studies with diabetic rats, which underwent bariatric procedures showed improved glucose tolerance and decreased fasting blood glucose.
• Type II diabetes continues to be associated with high rates of morbidity and mortality, leading to both financial and social burdens.
• Obese patients has normal blood glucose, glycosylated hemoglobin and insulin levels and fourfold increase in insulin sensitivity without continuation of diabetic medication 2 to 4 weeks after Bariatric surgery.
• Bariatric surgery is going to be more aggressive in the last five years and attempts to apply that kind of surgery even to patients with BMI of 30 kg/m2.
• Bariatric surgery for type 2 diabetes must be performed within accepted international and national guidelines. This requires appropriate assessment for the procedure and comprehensive and ongoing multidisciplinary care, patient education, follow-up and clinical audit, as well as safe and effective surgical procedures. National guidelines for bariatric surgery in people with type 2 diabetes and a BMI of 35 or more need to be developed and promulgated.
Read more